Dr. Panagiotis A. Paraschakis Interventional Neuroradiologist
Interventional Neuroradiology (INR), also known as Neurointerventional Surgery (NIS), Endovascular Therapy (EVT), Endovascular Neurosurgery, and Interventional Neurology, is a medical subspecialty of neurosurgery, neuroradiology, interventional radiology, and neurology. It uses endovascular catheter-based and image-guided techniques for the diagnosis and treatment of various neurovascular disorders of the head, neck, and spine. Although interventional neurology techniques have existed for decades, recent landmark trials in thrombectomy after stroke have become a cornerstone in the evolution of interventional neurology and neuroradiology.
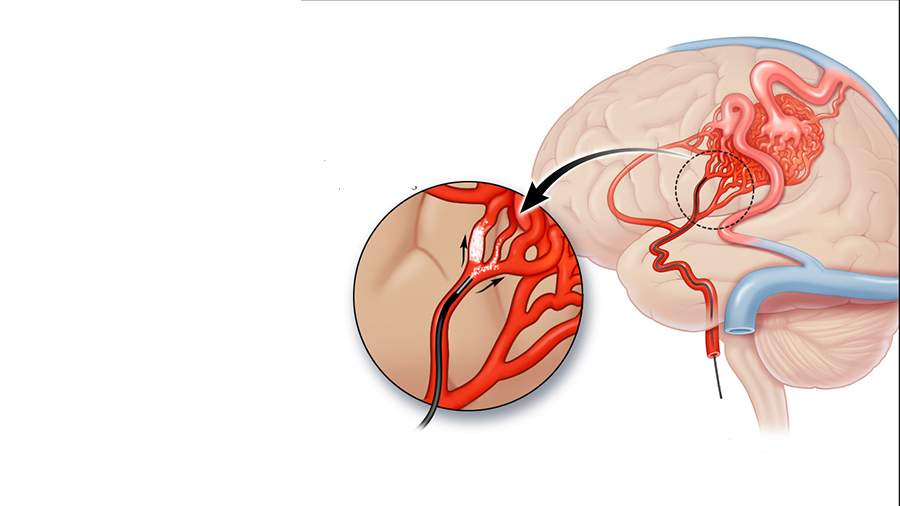
Imaging requires high-tech equipment for guiding the instruments used during the procedure. Thin tubes (catheters) and wires are inserted into blood vessels and directed to the affected area. Treatments, in the case of aneurysms or removal of blood clots, are delivered through these catheters. Diagnostic angiography forms the foundation of the field, upon which interventional procedures for the treatment of a variety of diseases are based and performed.
The benefits patients gain from this procedure are significant. A key advantage is reduced pain as well as shorter hospitalization and recovery time, due to the minimally invasive nature of the intervention. Otherwise, open surgery would be required. In addition, the use of advanced technology equipment ensures precise localization of the affected area and, consequently, better management of the problem.
Affiliated Hospitals
Affiliated Hospitals
Which vascular pathologies do we treat?
We focus on the treatment of brain aneurysms, ischemic strokes, arteriovenous malformations or fistulas of the brain and spinal cord, stenoses of the brain and neck arteries, chronic subdural hematomas, and stenoses of the cerebral venous sinuses.
Frequently Asked Questions
About Brain Aneurysm
What is a brain aneurysm?
An intracranial aneurysm, or brain aneurysm, is an abnormal bulging of the vessel wall that forms a sac. Inside this sac, blood circulates under pressure, which increases its fragility. The main risk is rupture, causing bleeding that most often accumulates in the coverings of the brain, the meninges.
Known risk factors for aneurysms, apart from heredity, include smoking, arterial hypertension, and excessive alcohol consumption.
How are aneurysms detected?
Aneurysms are often discovered incidentally during an imaging test (CT or MR angiography) performed for another reason. In other cases, they are revealed after their rupture, which causes a sudden and severe headache that may be accompanied by vomiting or neck pain.
How are aneurysms treated?
There are two types of therapeutic approaches for aneurysms.
The neurosurgical approach, in which the aneurysm is accessed through open surgery and isolated from the circulation using one or more clips.
The endovascular approach, in which materials are navigated through the arteries and metallic coils are placed inside the aneurysm, either alone or in combination with a stent. Alternatively, a special type of stent (flow diverter) can be placed in the artery carrying the aneurysm to redirect blood flow.
Do all aneurysms require treatment?
Aneurysms that have ruptured require urgent treatment. For aneurysms discovered incidentally, we assess their risk on a case-by-case basis, depending on their size, shape, location, as well as the presence of risk factors, and then recommend either treatment or monitoring.
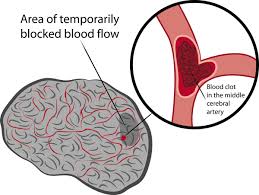
Ischemic Stroke (Cerebrovascular Accident – CVA)
Ischemic stroke is the leading cause of disability in the Western world. It is caused by the blockage of a brain artery, most often by a clot originating from the heart or the carotid arteries.
What are the symptoms?
Symptoms such as facial paralysis with drooping of the mouth corner, loss of strength or paralysis of the arm and leg on the same side, difficulty or inability in speech or understanding, loss of vision, loss of balance, unsteadiness, numbness, or loss of touch sensation may be signs of a stroke.
What actions need to be taken?
If we witness such an episode in a relative, friend, or even a stranger, we must immediately call an ambulance so that the patient can be transferred quickly to the hospital. There, specialists will evaluate the patient and refer them for further tests, such as a brain CT scan (CT, CT angiography). If an obstruction of a major vessel supplying the brain is found, the patient needs to undergo an interventional treatment.
What is the treatment for ischemic stroke?
There are two main therapeutic approaches when the necessary conditions are met. First, the intravenous administration of medication that can dissolve the clot (intravenous thrombolysis). However, greater effectiveness is achieved through interventional removal of the clot. This procedure is called mechanical thrombectomy. The sooner it is performed, the higher the chances that the patient will regain independence.
Which risk factors can be modified?
After an ischemic stroke, whether it has significant consequences for the patient or not, a complete cardiological evaluation must be carried out to rule out or treat cardiac conditions that could lead to another episode. The vessels supplying the brain (the carotid and vertebral arteries) as well as the major intracranial vessels (internal carotids, middle cerebral arteries, vertebral arteries, basilar artery) must also be examined.
Can arterial stenoses be treated?
If a stenosis in the arteries, either before or within the brain, is symptomatic (causing an ischemic stroke), it is highly likely that treatment is required. This can be performed endovascularly, where a balloon is used to open the artery at the site of the narrowing (angioplasty), and a stent is then placed.
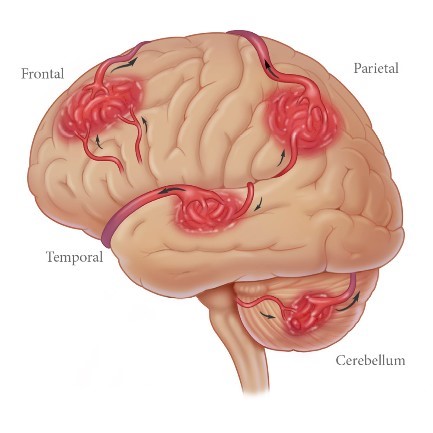
Arteriovenous Malformation (AVM)
It is an abnormal connection between arteries and veins, mediated by malformed vessels (nidus). This condition may be discovered incidentally (after an MRI or CT scan), following a seizure, or after a hemorrhage (intracerebral hematoma).
Frequently Asked Questions
About Arteriovenous Malformation (AVM).
What is the approach we follow for arteriovenous malformations (AVMs)?
When an arteriovenous malformation (AVM) is discovered incidentally, the next step is to perform a digital subtraction angiography (DSA brain) in order to identify its exact characteristics and assess its risk. If additional aneurysms or arteriovenous fistulas are found, treatment may be required. Otherwise, the usual approach is to monitor the AVM.
If the AVM ruptures, treatment is necessary within a period of 4 to 6 weeks after the episode.
How is arteriovenous malformation (AVM) treated today?
There are three different approaches to treating AVMs.
Endovascular treatment, where microcatheters are navigated through the arteries or veins to the site of the malformation, and a special liquid embolic material is used to block the abnormal vessels.
Open neurosurgical approach, where the malformation is accessed externally and isolated using clips or cauterization.
Radiosurgery, usually with a single dose of radiation (Gamma Knife / CyberKnife). This method works progressively over 3 to 5 years.
In some cases, a combination of treatment methods may be required, depending on the situation.
Arteriovenous Fistula (AVF)
This condition is characterized by a direct connection between an artery (or arteries) and veins. An AVF (fistula) may be discovered either incidentally or after a hemorrhagic event. In the first case, a digital subtraction angiography (DSA) of the brain is performed to classify the fistula and assess the risk of bleeding. If the risk is deemed high, we recommend treatment using the same techniques. In the case of hemorrhage, the intervention is performed in the acute phase.
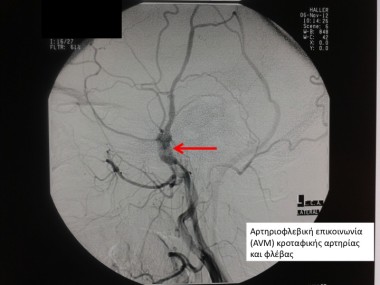
Where is an arteriovenous malformation (AVM) or arteriovenous fistula (AVF) located?
These conditions can occur throughout the body. The focus of neuroradiology, however, is the study and treatment of such vascular pathologies of the brain (intracranial) and spinal cord. When located in the spinal cord, they are characterized by progressive paralysis of the lower limbs.
Chronic Subdural Hematoma

This condition mainly affects patients over the age of 70 and refers to the accumulation of blood in the coverings of the brain, specifically beneath the dura mater. It usually involves recurrent episodes with a wide range of clinical presentations, from no symptoms to paralysis and cognitive disturbances.
What is the treatment for chronic subdural hematoma?
Treatment may involve either monitoring or surgical drainage. Recently, a new technique has been introduced—embolization of the middle meningeal artery—which has been shown to yield very positive results in accelerating the absorption time of the hematoma and reducing recurrences. As a result, additional surgical interventions are often unnecessary. Embolization can be performed in combination with surgical removal of the hematoma or as a standalone treatment.
Do you still have questions?
Email us for more information or for an evaluation of your test results.
Dr. Panagiotis A. Paraschakis Interventional Neuroradiologist
Dr. Panagiotis Paraschakis graduated from the Medical School of the Aristotle University of Thessaloniki. He obtained his specialization title in Diagnostic Radiology in 2016 in Athens.
He specialized in interventional neuroradiology at the Fondation Adolphe de Rothschild Hospital in Paris. He worked as a specialist at Hôpital Neurologique in Lyon and Hôpital Pasteur II in Nice.
Since May 2021, he has been working in Cyprus.
Since July 2025, he has been a trainer in Interventional Neuroradiology at the University General Hospital of Alexandroupolis.
